Telehealth trends are redefining the healthcare landscape in 2026, transforming how patients access care and how providers deliver it. From real-time virtual consultations to AI-enabled remote monitoring, telehealth is no longer a future concept — it’s the new standard.
While this shift has opened doors for many innovative healthcare startups, traditional healthcare providers often find themselves struggling to keep up with rapid advancements in telehealth technology. To stay relevant and competitive, established healthcare systems must upgrade their digital infrastructure and align with the latest telehealth trends of 2026.
But knowing which features to adopt and how much to invest can be overwhelming. That’s where choosing the right technology partner becomes essential — someone who understands the evolving digital health ecosystem and can guide your transformation journey.
Whether you’re a large healthcare organization or a small private practice, adapting to these changes is no longer optional. Fortunately, you don’t need to be a tech giant to succeed.
Our digital health experts have analyzed the most impactful telehealth trends shaping 2026 — from emerging technologies to regulatory shifts — to help providers like you make smart, future-ready decisions.
In this article, we break down the key trends, explore the tools driving them, and explain how healthcare providers can strategically leverage telehealth to enhance patient care, improve efficiency, and stay ahead of the curve.
7 Key Trends Driving the Future of Telehealth
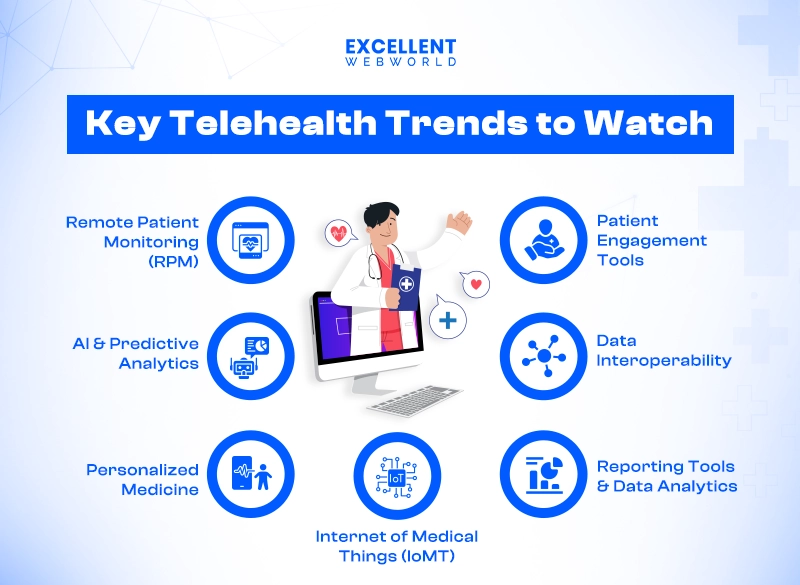
1. Remote Patient Monitoring (RPM) for Patient-Centric Care
Remote patient monitoring (RPM) is set to be one of the leading telehealth trends in the coming years. RPM enables healthcare providers to monitor from a distance. The complete process of monitoring is very time-saving and cost-effective. It will be done with the help of wearable or smart devices.
Key benefits of Remote Patient Monitoring:
What if AI could help connect you with the right medical care, exactly when you need it?
Health systems entrepreneur, surgeon and TED Fellow Mohamed Aburawi (@aburawiMD) explores how his digital health platform, Speetar (@SpeetarHealth), uses AI to bridge the healthcare gap in… pic.twitter.com/C4PXjmcExm
— TED Fellows (@TEDFellow) January 16, 2025
2. AI and Predictive Analytics are Here to Stay
AI will significantly impact diagnosis, treatment, and administration by accurately analyzing large amounts of data. For instance, AI helps identify abnormalities in radiology medical images, leading to earlier and more accurate diagnoses.
On the administrative side, AI can automate tasks like scheduling appointments and updating patient records, freeing up time for providers to focus on care. Predictive analytics combines AI with machine learning to anticipate patient needs and identify those at risk of complications after surgery or disease recurrence. Overall, AI will help deliver a more patient-centered approach across various specialties.
Key Benefits of AI and Predictive Analytics:
3. More Advancements in Personalized Medicine
Personalized medicine in healthcare tailors care plans based on each patient’s unique genetics, lifestyle, and environment. This feature is mostly adopted by many professionals who want to follow healthcare UI/UX design trends in their solutions. You can expect advancements like targeted therapies for diseases such as cancer, where treatment can be customized according to the patient’s profile. This precision medicine approach enhances treatment success rates while minimizing side effects.
Key Benefits of Personalized Medicine:
4. Enhanced Patient Engagement Tools
You can boost engagement, especially with AI-driven chatbots that can answer queries and guide patients to the right resources. These integrated chatbots in healthcare provide more control to patients by accessibility and responsiveness.
Key Benefits of AI-Driven Chatbots:
5. Data Interoperability Moves Forward
Efficiently sharing data among healthcare providers is essential for coordinated care. Advances in health information exchange (HIE) platforms and adopting FHIR (Fast Healthcare Interoperability Resources) standards are improving data interoperability. By 2026, more organizations will be able to share patient records seamlessly.
Key Benefits of Data Interoperability:
6. Advanced Reporting Tools and Data Analytics
Healthcare providers rely on performance metrics to make better decisions about patient care. Advanced reporting tools are expected to follow trends in telehealth to offer insights into administrative processes, patient outcomes, and financial health by compiling data from various sources for a holistic view.
For example, analytics helps you to reduce waiting time.
This information allows practices to make data-driven adjustments that enhance patient satisfaction.
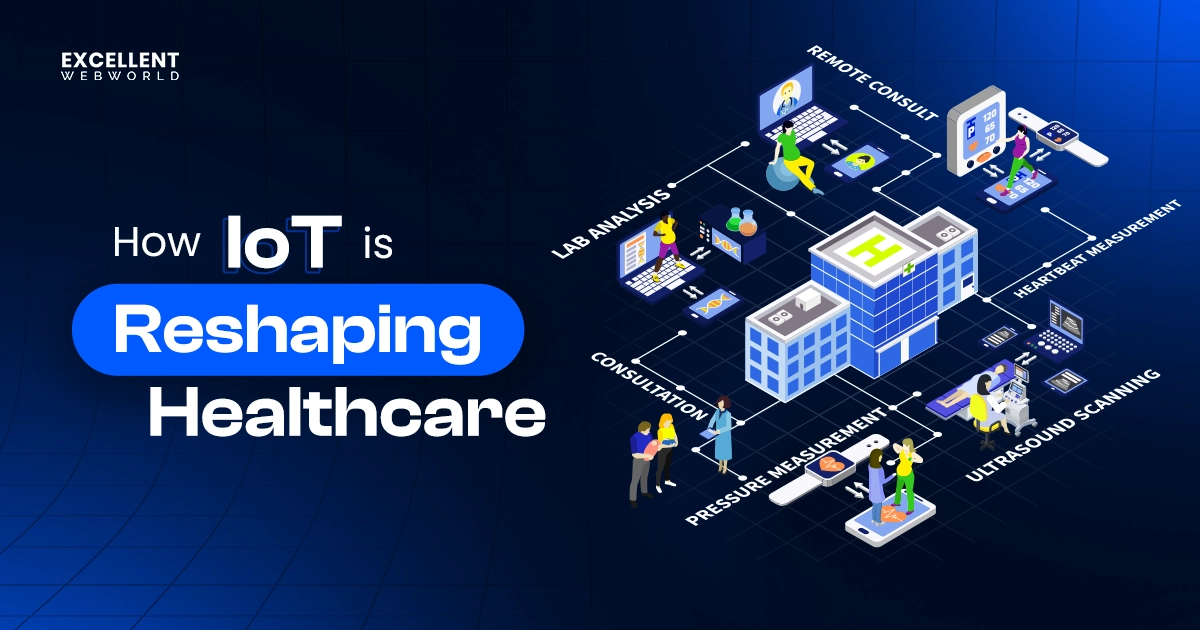
7. Internet of Medical Things (IoMT)
IoMT devices like smart inhalers and wearable ECG monitors help to grow at a 20.4% CAGR from 2023 to 2030 as providers adopt these technologies for better remote monitoring and preventive care.
IoMT enables continuous data collection that informs diagnoses and interventions while giving patients greater control over their health outcomes. This promotes engagement and proactive health management.
Key Benefits of IoMT:
Telehealth Trends Our Experts Are Predicting
Healthcare providers are adopting hybrid models that mix in-person visits with online care. As regulation compliance evolves to support virtual healthcare and the rising importance of telemedicine, you can anticipate more standardized practices and broader insurance coverage. Our experts, with years of experience working closely with various healthcare organizations. With this experience, our team is well-positioned to predict these trends.
Our team has seen firsthand how advancements in technology and changing patient needs shape the future of telehealth, allowing us to provide valuable insights into what lies ahead in this dynamic landscape.
Here are some of the key telehealth future trends,
1. Increased AI Integration
The rise of AI is a significant trend in telehealth that will benefit the entire medical field. Telemedicine focuses on efficiency and data management and is poised for substantial transformation. One prominent area of growth is virtual nursing assistants, which are projected to represent 26.4% of all AI revenue in telehealth.
Sophisticated AI chatbots can swiftly engage patients regarding their symptoms and link them to doctors, offering 24/7 support. They may even assist by taking notes for healthcare providers, expediting the diagnostic process.
AI integration services provide assess vital data for early indications of health problems, fostering more personalized care and improved health outcomes. AI integration is exciting for the healthcare industry because it can transform mental health forever!
Medical practitioners can use AI to offer virtual counseling services. Mental health chatbots and virtual consultations, which are always accessible, can transform patients’ care.
2. Greater Support for Wearables
Wearable devices and telemedicine apps for doctors and patients are expected to advance in 2026. Wearables provide real-time data that enhances care. The market shows confidence in growth, especially after the FDA approved smartwatches as a medical device development tool (MDDT) in May 2024.
These devices can now be utilized in clinical trials and symptom tracking, enhancing the accessibility of telehealth services. For example, the wearables in telehealth solutions can help track key symptoms like diabetes-related foot disease.
The Potential Role of Sensors, Wearables and Telehealth in the Remote Management of Diabetes-Related Foot Disease https://t.co/b3N9Zna3wI @jcu @keckmedusc @usc #DiabeticFoot pic.twitter.com/QggfFxEBlC
— David G. Armstrong (@DGArmstrong) February 13, 2024
3. Legal Challenges to Expanded Coverage
Several Medicare restrictions will return, limiting telehealth coverage to rural areas lacking healthcare professionals. Patients who need telemedicine still have coverage, but those who prefer virtual care may find their options reduced.
Mental health services typically have no geographic restrictions and still receive support from private insurers. However, these new limitations could slow the rapid growth of telehealth platforms that have recently been experienced.
What Are The Benefits Of Telehealth As A Technology Trend?
Telehealth has become a game-changing healthcare trend, changing how patients and providers connect. It helps make healthcare more accessible while maintaining quality, using digital technology to provide smooth and remote healthcare services.
Benefits Of Telehealth For Patients:
1. Better Patient Outcomes
Telehealth is particularly effective for treating chronic conditions like high blood pressure and heart disease. There is no need to visit hospitals or clinics for check-ups. The patient can connect with healthcare professionals virtually, which helps reduce missed appointments.
2. Medical Care Within Reach
Patients need to visit healthcare professionals safely and comfortably, and the best possible way is to do so virtually and get medical help from home through telehealth.
3. Increased Engagement
After telehealth technology emerged, accessing healthcare has become much easier for patients. This accessibility allows patients to engage quickly and effectively with healthcare professionals.
4. Affordable and Timely Healthcare
High medical costs used to be a significant barrier in healthcare. However, telehealth has transformed medical practices and cut costs. Telehealth helps patients with more affordability and prompt diagnoses.
5. Fewer Hospital Readmissions
Telehealth makes it easier for patients with mobility issues or disabilities. Patients get care without traveling to clinics or emergency rooms. Those requiring long-term care can receive assistance from home. Patients need to follow instructions and manage medications without the expense of hospital stays.
Benefits Of Telehealth For Providers
1. Improved Clinical Outcomes
Telehealth has made it easier for healthcare professionals to track patients consistently and catch health issues timely. This digital tracking outperformed traditional in-person care for better clinical outcomes.
2. Lower Mortality Rates
Remote ICUs significantly decreased the mortality rate. More than 20 studies indicate fewer complications and deaths after implementing these remote care systems.
3. Consistent Medical Support
Fields like behavioral therapy must be tracked regularly to prevent risky behavior changes. Telehealth made it easy to access support and monitoring for patients. This ensures they receive the help on time.
What Are The Pros And Cons Of Telehealth?
Telehealth has become popular as a modern way to address healthcare challenges, providing accessibility and convenience. However, like any tech-based service, it has its benefits and drawbacks.
Pros Of Telehealth
1. Convenience and Accessibility
A study by Cisco shows that 74% of patients favor simple access to medical care services rather than visiting hospitals or clinics.
Telehealth ends the appointment barriers for patients; taking the day off from work to consult is unnecessary. Additionally, telemedicine can help with tests and virtual consultations if a patient suffers from a chronic disease.
2. Time Saver
Telehealth saves time in consultation, tests, and medications; even a report says it will take 121 minutes to consult a doctor, including travel, waiting, and actual consult time. So, telehealth decreases the time needed to complete the process and makes it faster and more accurate.
3. Easy Follow-Up
Telehealth made follow-ups easy, whether it was post-medical procedures or ailments. This helps patients, especially for those who need rest after treatment. Virtual visits provide easy follow-up and comfort.
Cons Of Telehealth
1. Limited Scope
Telehealth is mainly used for initial consultations and follow-up meetings. For instance, a doctor can’t physically examine a patient during a virtual visit, which limits the effectiveness of the consultation. While telehealth is suitable for minor discussions, it can’t fully replace the thoroughness and reliability of traditional in-person appointments. There are also concerns about accuracy; although a healthcare professional can assess a condition virtually, it’s often difficult to gauge its seriousness without a physical examination.
2. Requires Smart Devices
Both patients and doctors need reliable internet connections and devices that support telehealth services. While healthcare practices usually have access to these tools, patients may struggle if they can’t afford or borrow a device. This requirement can limit some individuals’ access to telehealth services.
3. Requires Internet
Internet access is crucial for telehealth; consultations can’t happen without it. Although some discussions can occur over the phone, most require visual assessments from the doctor. Unstable internet connections can disrupt appointments; if the patient or doctor loses connection, the entire visit can be halted, leading to delays or extended wait times.
How Can Excellent Webworld Help You With Telemedicine Technologies?
The above article must have helped you to understand telemedicine technologies and telehealth industry trends. However, When considering how to develop a telemedicine app, one of the critical aspects is understanding the nuances of the healthcare industry. Excellent Webworld is an experienced telemedicine app development company with domain expertise, helping you navigate complex regulatory requirements like HIPAA, GDPR, and PIPEDA to safeguard patient data and build trust.
We have over 13 years of experience delivering telemedicine app development services for clinicians, medical practitioners, and hospital chains. Our team of experts has successfully delivered high-performance telemedicine apps integrating advanced IoT and AI technologies. With more than 900 successful projects, our experts have been catering to different client needs in the healthcare industry.
We are a leading telehealth app development company that offers end-to-end IoT development and integration for medical practices. Contact us now to consult our IoT experts and work with a team known for its expertise in healthcare app development services that support secure and scalable patient solutions.
Why Choose Excellent Webworld’s Dedicated Team Over In-House Developers?
By choosing Excellent Webworld’s dedicated team, you can access a pool of skilled professionals without the overhead of hiring in-house staff or the irregularity of freelancer developers.
This dedicated team offers perfect expertise, reliability, and scalability, ensuring seamless collaboration and high-quality results.
| USPs | In-House | Excellent Webworld | Freelancer |
|---|---|---|---|
| Weekend Support | No | Yes | No |
| Dedicated Resources | Yes | Yes | No |
| Termination Cost | High | No | No |
| Project Manager Cost | High | No | No |
| Query Support | High | 24×7 | No |
| Time to Start Project | 2 – 10 Weeks | 1 Day – 2 Weeks | 1 – 10 Weeks |
| Hiring Model | Full Time | Monthly, Part & Full Time | Weekly, Hourly |
| Cost of Training | 10k – 30k USD | 0 | 0 |
| Time to Scale Size of the Team | 4 – 16 Weeks | 48 Hours | 1 – 10 Weeks |
| Availability | 8-9 hours (Depending on working hours) | Around-the-clock | Uncertain |
| Agile Development | Maybe | Yes | No |
| Free Trial | No | 7 Days | No |
FAQs
Telehealth reduces costs by minimizing physical infrastructure needs, optimizing resources, and lowering patient expenses like travel and time. It also enhances preventive care, reducing costly emergency treatments and hospital readmissions.
Telehealth apps safeguard patient data with encryption, secure authentication, and compliance with privacy regulations like HIPAA and GDPR.
Telehealth covers many digital health services, while telemedicine focuses on remote clinical care like diagnosis and treatment.
Telemedicine is the future of healthcare because it enhances accessibility, reduces costs, and improves efficiency by leveraging digital tools for remote diagnosis, treatment, and patient management.

Article By
Mayur Panchal is the CTO of Excellent Webworld. With his skills and expertise, He stays updated with industry trends and utilizes his technical expertise to address problems faced by entrepreneurs and startup owners.